Chinese acupuncture
Effective treatment by Chinese acupuncture includes making a diagnosis according to the teachings of Traditional Chinese Medicine. Diagnosis is made through various methods, such as assessment of facial color, appearance of the tongue, nature of the pulse beat, medical history, and even the occurrence of sweating.
Palpation, olfaction, hearing and vision are used to determine the condition of Qi and any patterns of disturbance. This Chinese diagnosis is considered as the basis for creating a holistic treatment strategy. It may include Chinese acupuncture and also herbal therapy or dietary changes.
Chinese acupuncture is considered to be much more effective than the still often practiced “Western” acupuncture, which provides treatment based on Western diagnoses.
A Chinese diagnosis is an essential prerequisite and the foundation for Chinese acupuncture.
The way to a diagnosis in Chinese medicine is fundamentally different from the procedure in today’s Western medicine. The doctor uses his senses to diagnose the patterns of disturbance of the vital energy Qi in the individual meridians and organs based on the symptoms, the disturbed functions of organs, the external appearance of the patient and the external examination.
The findings resp. the symptoms of a dysfunction or a disease are analyzed according to 8 classical diagnostic categories heat – cold, fullness – weakness, outside – inside, yang – yin. This is how a diagnosis is made in the Chinese sense.
Since the time of the Han dynasty (202 v. u.Z. – 220 n. u. Z.) Chinese doctors use 4 classical examination methods, Chinese Si jian.
The 4 methods of examination are:
- 1. Viewing, seeing (Wang),
- 2. Listening resp. Smelling (Wen),
- 3. Inquiry (Wen),
- 4. Examination, palpation (Qie).
Some examination methods were the focus of attention, such as looking at the color of the skin, examining the tongue, as well as feeling the pulse. The classification of specific symptoms and findings into the classical categories of disharmony has become more and more refined. The holistic approach, as well as the intuitive grasp of disturbance patterns, was given great attention in the diagnostic procedure.
Chinese acupuncture – Some examples of diagnostic procedures
The Chinese physician attaches particular importance to observation Assessment of the Shen of the patient. Shen, the spirit, the psychic energy, is essentially revealed in the glow of the eyes. The expression of the face and the clarity of the thoughts are also an important indication of the state of Shen. It is said the “patient has Shen.
In the case of weakness of Shen, the eyes are dull, without luster, the facial expression is unresponsive, the thoughts are disjointed and without persuasion. Since Shen depends on Qi and Blood, a weakness of Shen indicates a disturbance of Qi and Blood.
Also Color of the face is assessed. It gives important clues about the state of Qi and blood in the organs. The colors are assigned to the organs according to the theory of the five phases of change.
A “white face”, i.e. paleness, indicates a general tendency to cold disorders or. a weakening disorder. also in chronic lung diseases one finds pronounced pallor and often “colorlessness” of the face. Gray, “black” complexion indicates weakness of Kidney energy. Grayish skin coloration often occurs under the eyes.
Yellowish-green facial color is indicative of liver disease, while yellowish-brown color indicates digestive dysfunction of the spleen-pancreas system. Red color of the face is typical in heart diseases and can also occur in heat disorders.
The Observation of the tongue Chinese medicine pays special attention to this problem. In addition to size and consistency, the color of the tongue and the tongue coating play an important role.
A pale tongue indicates a weakening or. cold disturbance, while a more reddened tongue indicates heat disturbances of the internal organs. Dry tongue is an indication of heat disorder resp. Yin weakness, a very moist tongue indicates cold disturbance.
The functional circle spleen-pancreas and stomach determines the quality of the tongue coating. A small amount of tongue coating can be a normal. A thick coating is an expression of a state of fullness, if very dry or shrunken Indication of heat and thus loss of yin forces, i.e. yin weakness.
Yellowish coating indicates heat disturbance. White watery coating occurs in the case of fullness or. Heat of the stomach before. A swelling or enlargement of the tongue with tooth impressions is characteristic of spleen-pancreas disorders.
The traditional therapist asks the patient about his medical history, the course of previous and current disorders or. Diseases and also evaluates them according to the 8 diagnostic categories. Chronic illnesses indicate a weakening of the organs, acute illnesses usually indicate filling disorders.
Often medical history shows recurrence of certain organ weaknesses. Thus, the same disturbance patterns can often recur in different diseases.
Furthermore, the reaction of the patient to cold or. heat, as well as the character and exact localization of the pain is asked for.
Sudden and frequent Sweating even after minor exertion are signs of yang weakness. Night sweats indicate a weakness of Yin with accompanying Yang fullness.
Excessive Thirst is a typical heat or. Yang symptom, where Yin fluid is depleted. ravenous hunger or. excessive appetite are an expression of a weakness of Qi. Lack of appetite with abdominal fullness indicates weakness of the stomach and spleen-pancreas functional circuits.
Constipation in elderly people or after a long illness, weakness of Qi and “consumption” of body fluids occur. Spastic constipation is an abundance or. Yang disorder of the digestive system.
Pain are, according to Chinese belief, due to disturbances in the flow of vital energy, i.e. qi. Acute pain or cramps are attributed to blockage of qi with fullness. Dull pressing or drilling pains are often caused by a weakness of Qi.
Since pain is often the symptom from which the patient suffers the most, the analysis of pain according to the criteria of Chinese medicine is crucial for the subsequent therapeutic procedure. Often radiating Pain along meridians out, so z. B. Heart pain in angina pectoris along the heart meridian.
Also external illnesses co-caused by cold or wind, such as z. B. Ischialgia or cervical spine syndrome along certain meridians. It is said that the Qi of the meridian is stagnated.
The assignment of pain to the corresponding meridians is decisive for the later point selection in therapy. If headaches are localized in the gallbladder meridian area of the head, treat with distant points of the gallbladder meridian on the leg and foot. In addition to the localization of pain, the quality of the pain and the changes in pain sensations are decisive for the diagnosis.
The Chinese diagnoses are known in the West as Chinese syndromes called in the traditional sense. Here are some examples Weakness of Lung-Qi, Weakness of Kidney-Yang, Rising Liver-Fire, Weakness of Heart-Qi. Syndromes in this sense means not only the sum of symptoms, but also their energetic cause and interpretation according to the ideas of the Chinese medical system.
After a Chinese diagnosis has been made, a therapy strategy is determined in the second step z. B. the intention to strengthen the Qi of the lungs or to harmonize the ascending liver energy. In the case of combined Chinese syndromes, several therapeutic strategies may be necessary.
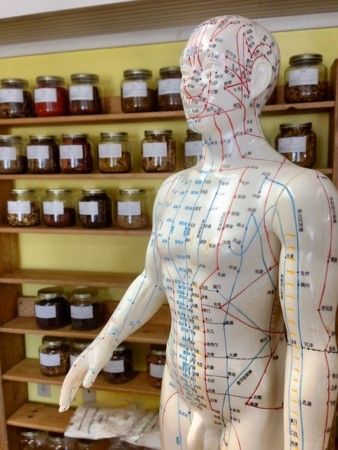
From the therapeutic strategies, the third step of a Chinese acupuncture results in certain effective point combinations for Chinese acupuncture therapy, which are then applied in the individual acupuncture sessions.
Accompanying behavioral measures or a change of diet according to the 5 elements are also recommended, which are helpful in this pattern of disturbances. In the case of deeper organ disorders, the administration of Chinese medicinal herbs can be useful.
From the Chinese diagnosis follow primary therapy strategies as well as the determination of optimal point combinations for needling.
Western acupuncture
The Chinese acupuncture is used by ca. Applied by 20% of acupuncturists in the West, the majority of physicians practice a Western form of acupuncture.
This is primarily based on western diagnoses and on disease concepts of western medicine, as they are common in the application of medicines, without taking into account the basic energetic conditions of the diseases. In the case of pain, z. B. instead of diclofenac or aspirin, pain-relieving points such as colon 4 or stomach 44 needled.
Especially in chronic diseases this western symptomatic acupuncture is not very effective because it does not take into account the underlying energetic disturbance patterns, i.e. the Chinese diagnosis. This form of acupuncture application does not lead to permanent improvement or cure.
It shows only a short-term relief of symptoms, similar to Diclofenac also only works for a short time and must be taken over and over again. In chronic diseases such as migraine, tinnitus, depression, sleep disorder, trigeminal neuralgia, the success of acupuncture treatment depends on the preceding Chinese diagnostic classification of the disease. Also the consequent consideration of the developed therapy strategies is of essential importance.
Patients are advised to inquire about the duration of training of their therapist and also about the experience in the application, i.e. for how many years acupuncture has been practiced and with what frequency in the specific clinical picture.